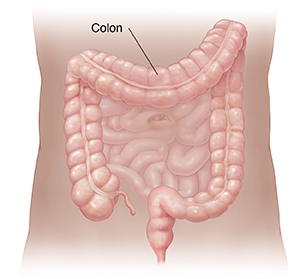
Colitis is when a part of your colon becomes inflamed or swollen. The colon is also called the large intestine. It helps with digestion and waste removal.
What causes colitis?
Colitis can be caused by many things. The most common causes are:
-
Viral or bacterial infections
-
Inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
-
Certain medicines, such as antibiotics
-
Radiation therapy to the colon
Symptoms of colitis
The symptoms of colitis may last a short time. Or they can be chronic. The most common symptoms are:
-
Diarrhea, sometimes bloody
-
Stomach pain or cramping
-
Fever
-
Weight loss in severe cases
Diagnosing colitis
Your healthcare provider will take a full health history and family history. They will also give you a physical exam. Depending on the results of your history and physical exam, your provider may also order certain tests to help find out the cause of your colitis. These may include:
-
Lab tests. Your blood and stool will be checked.
-
Endoscopy and biopsy. Endoscopy is a procedure that uses a long, flexible tube with a tiny light and camera on one end to check the inside of your large intestine. Two types of endoscopy are sigmoidoscopy (view lower colon) or colonoscopy (view entire colon). During an endoscopy, your provider may take a small sample of your tissue to look at under a microscope. This is called a biopsy.
-
Imaging tests. These include X-ray, CT scan, MRI, and capsule endoscopy.
Treatment for colitis
Treatment for colitis depends on what is causing it and how serious your symptoms are. In some cases, you may not need treatment. For example, colitis from an infection may go away without care.
Treatment may include:
-
Medicines. You may take these by mouth (oral) or as a rectal suppository or enema. Some medicines are given by injection. They can lessen swelling and ease symptoms.
-
Changes in your diet. Some foods can make symptoms worse. Common triggers are milk, coffee, alcohol, and fried foods. Talk with your healthcare provider to develop a healthy diet plan.
-
Surgery. In some cases, you may need surgery to remove a damaged part of the colon.
Call 911
Call
-
Trouble breathing
-
Confusion
-
Very drowsy or trouble awakening
-
Fainting or loss of consciousness
-
Rapid heart rate
-
Chest pain
When to call your healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Symptoms that don’t get better, or get worse
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Pain that gets worse
-
Bloody diarrhea
-
Bleeding from your rectum
-
New symptoms
Author: Semko, Laura
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.